One in two women and one in five men over the age of 50 in the U.K. will break a bone because of underlying osteoporosis.
BBH - Border Bone Health UK
Our bones can be normal and strong, osteoporotic and fragile or somewhere in between. Skeletal bones are made up of a thick outer shell surrounding a strong inner mesh consisting of collagen, calcium salts and minerals. In the spaces between the inner supporting struts of bone are blood vessels and bone marrow. Bone is alive and constantly changing. Old, worn out bone is broken down by cells called osteoclasts and is then built up again by bone building cells called osteoblasts. This process is known as bone turnover. Up until the age of 35 there is a balance between bone break-down and new bone formation which means that bone density remains stable. After this age bone loss increases as part of the normal ageing process. However this can lead to Osteoporosis and an increased risk of fracture.
Osteoporosis means that some of the struts of bone become thin or break and the bone becomes too porous. Osteoporosis may make a person more prone to a bone fracture which can follow from a fall or more rarely can occur spontaneously. Any bone may be affected, but the most common fractures involve the hip, wrist or the spine. Fractures resulting from bone fragility in the elderly have a major impact on quality of life and frequently cause serious disability.
Peak bone mass is achieved by age 30. Genetics or lifestyle factors (Poor diet or excessive dieting, lack of exercise, illness) may mean that a good bone density is not achieved. Low peak bone mass becomes a disadvantage in old age. After skeletal maturity, bone is lost in both women and men at about 1% a year. Women experience a phase of accelerated bone loss for three years after the menopause.
Risk Factors or Warning Signs of Osteoporosis
Osteoporosis is silent in its early stages; a broken bone is sometimes the first indication that a person has Osteoporosis. There are changes in the body that can indicate Osteoporosis is developing, and should be brought to your doctor's attention:
Bone fractures after age 50
Change in posture; becoming more hunched forward 'Kyphosis'.
Sudden back pain.
Loss of height.
Additional risk factors include:
Being a post-menopausal woman.
Low Testosterone in males.
Having a small, slight body frame.
A family history of Osteoporosis.
Being of Caucasian, Asian, or Latino heritage.
A diet low in Calcium and Vitamin D.
Inactivity—exercise strengthens bones.
Smoking, either past or present.
Consuming large amounts of alcohol.
Use of Corticosteroids.
Certain conditions and treatments can put you at higher risk of developing Osteoporosis, so people who have any of the conditions on this list should consider getting an Osteoporosis screening:
Endocrine conditions such as Diabetes, Hyperthyroidism, or Hypothyroidism.
Autoimmune disorders such as Rheumatoid Arthritis.
Digestive conditions like Celiac and Crohns disease.
Weight loss surgery.
Haematologic or blood disorders such as Lymphoma or Leukaemia.
Men and Women who have had Bulimia or Anorexia.
Ages - Adults age 50+
40+ with risk factors.
Younger that 40yo in rare circumstances, past/present high risk factors such as Anorexia Nervosa and Bulimia.
Frequency - Bone density screening can be conducted annually.
C.U.B.A.CLINICAL has a minimum threshold for scanning and analysis set at 20 years old.
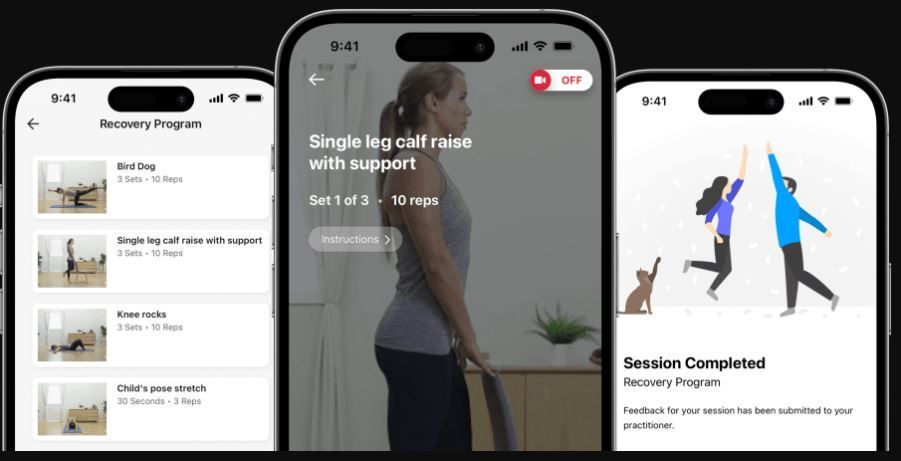
COMING SOON
Get ready. Get set.
Many new services, features, health, and digital health initiatives...
One such initiative is the digital exercise program for exercise on prescription.
Watch this space!